Need to contact or place a phone call to NationsOTC: 877-239-2942 (TTY: 711)
Contact Line for Current Members: Please first call the number found on the back of your member ID card for accurate and faster service.
ConnectiCare has been considered as the leader in health plan in the state of Connecticut for almost 40 years. ConnectiCare is known for their remarkable commitment to customer service, their connection with different doctors and hospitals, as well as their variety of health plans and services for the residents of Connecticut — their families, businesses, and municipalities. Being a part of EmblemHealth, ConnectiCare provides state, regional, as well as national networks of care for their customers and their members.
ConnectiCare, Inc. is an HMO/HMO-POS plan that has a Medicare contract. ConnectiCare Insurance Company, Inc. is an HMO D-SNP plan that has a contract with Medicare as well as a contract with the Connecticut Medicaid Program.
Every individual has different needs which is why ConnectiCare has a vast selection of Medicare Advantage plans that will provide their members the benefits they require at an affordable price. The following plans offer benefits that the Original Medicare does not offer:
- 2021 ConnectiCare Choice Part B Saver (HMO)
- 2021 ConnectiCare Flex Plan 3 (HMO-POS)
- 2021 ConnectiCare Choice Dual (HMO D-SNP)
- 2021 ConnectiCare Choice Dual Basic (HMO D-SNP)
These plans provide other benefits like:
- Wellness programs
- Fitness
- Teladoc
- Worldwide Emergent/Urgent Care
- Foot Care
- Foot exams and treatment
- Occupational, Speech, and Language Therapy
- Over-the-Counter Benefit
- And many more!
What is the ConnectiCare Medicare Advantage Over-the-Counter Benefit?
This is a program that will enable you to acquire over-the-counter items that will arrive at your address in the mail. The card must be activated and the initial OTC dollar amount will be loaded onto the card. This benefit will also assist you with the cost of essential health care products that are not within the medical or pharmacy expense under your plan. To add to this, it can aid you in saving money on a vast array of generic branded health essential products like cold medicines, pain relievers, dental care, first aid supplies, and so much more.
Advantages of using OTC benefit:
No additional costs!
If you will use the credit or pre-determined allowance that is provided within this benefit, all products you wish to get will be given to you at no extra cost. Your orders will also be delivered to your home without worrying about shipping fee as these will all be covered by the benefit.
ConnectiCare Medicare Advantage works with NationsOTC that will enable their members to purchase common everyday medical and personal health care essentials. Their team of clinicians, researchers, engineers, financial experts, and a great number of direct sales representatives have outstanding expertise and know everything about healthcare business.
The following are the common medical and personal care items that they offer for their partners:
- Eye and Ear Care
- First aid supplies
- Allergy sprays and gels
- Skin and sun care products
- Cold and flu products
- Dental and Denture Care
- Antacids and Acid Reducers
- Vitamins and Minerals
- And so many more!
These OTC products are all given to members at no extra cost. A credit or pre-determined allowance is given within the benefit. Shipping fee will not be charged to the member especially if this is inclusive in your plan. Find below the easy methods where active members of this program can submit their orders:
- They may scroll down below and go through on how to set up an account online. This is considered to be the fastest, most convenient, and easiest way to order 24/7.
- They may place their orders by calling 844-432-4327, TTY: 711
- They may send in a completed order form that is included in the catalog and mail it to the address indicated on the form.
How to know if a member is qualified?
Members must make sure to review the Summary of Benefits of their existing personal plan to verify if their plan has this benefit included in it. If it does, members must also be aware of the plan’s specified OTC allowance frequency, whether it is provided monthly or quarterly. The allowance amount may vary depending on the plan. The number to contact is given at the start of this article if you need further information about your plan benefits.
There are a few plans that are inclusive of an allowance that is provided on a monthly basis. These credits may be consumed to purchase some over-the-counter medications and supplies, comprising of digestive health treatments, allergy medication, pain relievers, first aid supplies, and so many more. Members must review the Evidence of Coverage of their plan to check if it is included in their benefit and to find out the exact amount of the monthly allowance provided.
IMPORTANT: Go directly to the site to confirm and acquire more information.
NOTE: The information provided here is not a comprehensive explanation of the benefits available to you. It is always best to communicate directly with the company to know more information about their available plans.
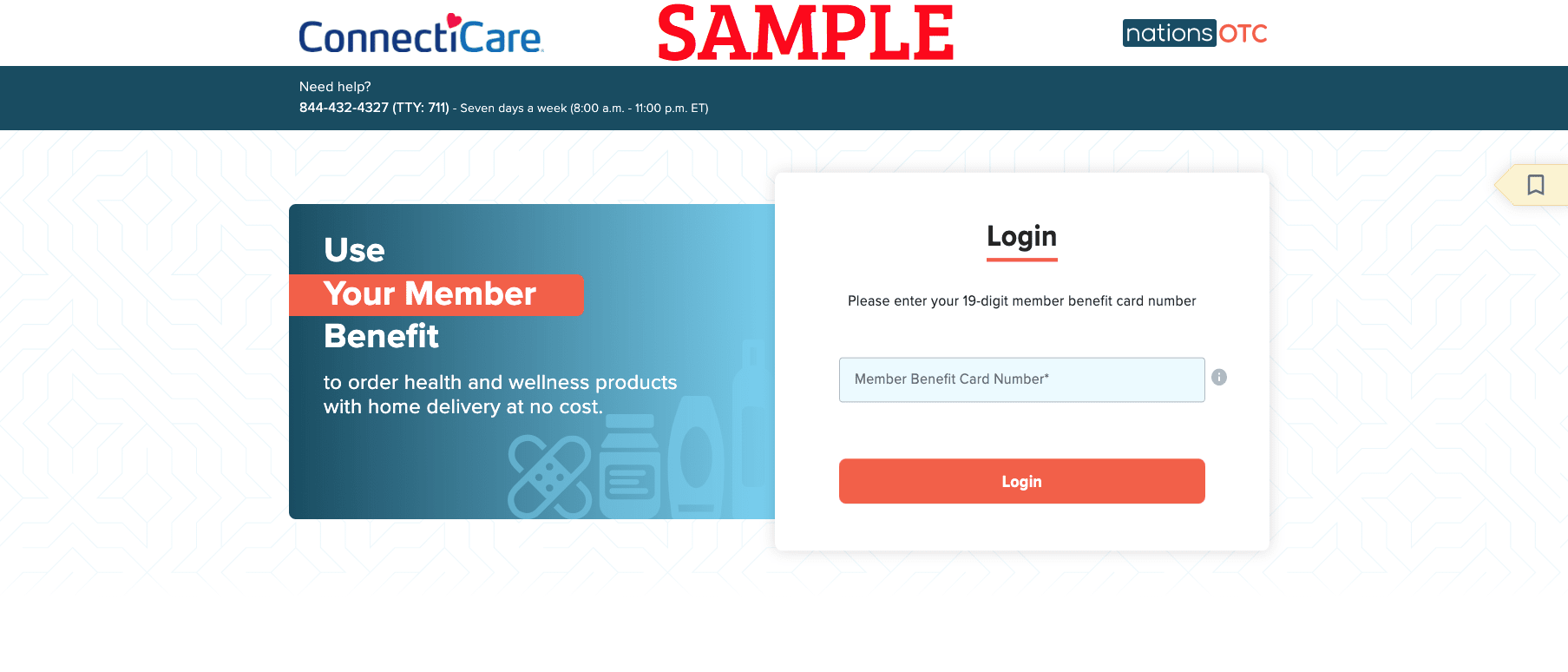
Easy-to-follow steps are provided below should you feel the need to access the login or registration page. A brief guide is available for you so you can discover how you can login or activate a new online account and gain access. Just make sure your personal information is close by.
Requirements to have available to be able to sign in or register to your ConnectiCare Medicare Advantage OTC account online:
- Stable internet access
- Email address
- Member information
- Personal information
Easy steps to follow for new cardholders who wish to activate their OTC card online:
- Visit link in your preferred search engine on your device.
- Type in your 19-digit card number in the space provided.
- Select the red “LOGIN” button to move forward.
- Continue to move forward and provide all the necessary information to complete the activation.
Valuable guidelines for creating / processing / submitting your order:
- The benefit is intended for the member’s use only. Using the benefit to purchase OTC items for friends and/or family is strictly prohibited.
- Delivery Time: Please allow 2-5 business days for your items to be shipped to your address.
- Return Policy: Due to the personal nature of the products, returns are not allowed.
You may download Aetna Medicare OTC Catalog:
NOTE:
If you wish to download the catalog, you may visit the link below:
2021 ConnectiCare Over-the-Counter Medications and Products Benefit Catalog and Order Form
Important information to take note of:
- If you are ordering by mail, you have to make sure that you follow the instructions to complete the order form. You have to mail it to the address indicated on the order form included in the catalog.
- If you have further questions about your plan, it is best to directly contact the following numbers: 1-800-224-2273, TTY: 711
ConnectiCare Medicare Advantage OTC Over-the-Counter Video Summary:
Want to view more articles on this topic? Click here to search our article database.